Buformin
 | |
| Clinical data | |
|---|---|
| Routes of administration | Oral |
| ATC code | |
| Pharmacokinetic data | |
| Excretion | Renal |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.010.662 |
| Chemical and physical data | |
| Formula | C6H15N5 |
| Molar mass | 157.221 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Buformin (1-butylbiguanide) is an oral antidiabetic drug of the biguanide class, chemically related to metformin and phenformin. Buformin was marketed by German pharmaceutical company Grünenthal as Silubin.
Chemistry and animal toxicology
[edit]Buformin hydrochloride is a fine, white to slightly yellow, crystalline, odorless powder, with a weakly acidic bitter taste. Its melting point is 174 to 177 °C, it is a strong base, and is freely soluble in water, methanol and ethanol, but insoluble in chloroform and ether.[1][2] Toxicity: guinea pig LD50 subcutaneous 18 mg/kg; mouse LD50 intraperitoneal 140 mg/kg and 300 mg/kg oral.[3] The log octanol-water partition coefficient (log P) is -1.20E+00; its water solubility is 7.46E+05 mg/L at 25 °C. Vapor pressure is 1.64E-04 mm Hg at 25 °C (EST); Henry's law constant is 8.14E-16 atm-m3/mole at 25 °C (EST). Its Atmospheric -OH rate constant is 1.60E-10 cm3/molecule-sec at 25 °C.[4]
Mechanism of action
[edit]Buformin delays absorption of glucose from the gastrointestinal tract, increases insulin sensitivity and glucose uptake into cells, and inhibits synthesis of glucose by the liver. Buformin and the other biguanides are not hypoglycemic, but rather antihyperglycemic agents. They do not produce hypoglycemia; instead, they reduce basal and postprandial hyperglycemia in diabetics.[5] Biguanides may antagonize the action of glucagon, thus reducing fasting glucose levels.[6]
Pharmacokinetics
[edit]After oral administration of 50 mg of buformin to volunteers, almost 90% of the applied quantity was recovered in the urine; the rate constant of elimination was found to be 0.38 per hr. Buformin is a strong base (pKa = 11.3) and not absorbed in the stomach. After intravenous injection of about 1 mg/kg buformin-14-C, the initial serum concentration is 0.2-0.4 μg/mL. Serum level and urinary elimination rate are linearly correlated.[7] In man, after oral administration of 50 mg 14-C-buformin, the maximum serum concentration was 0.26-0.41 μg/mL. The buformin was eliminated with an average half-life of 2 h. About 84% of the dose administered was found excreted unchanged in the urine.[8] Buformin is not metabolized in humans. The bioavailability of oral buformin and other biguanides is 40%-60%. Binding to plasma proteins is absent or very low.[9][10][11]
Dosage
[edit]The daily dose of buformin is 150–300 mg by mouth.[12] Buformin has also been available in a sustained release preparation, Silubin Retard, which is still sold in Romania.
Side effects and contraindications
[edit]The side effects encountered are anorexia, nausea, diarrhea, metallic taste, and weight loss. Its use is contraindicated in diabetic coma, ketoacidosis, severe infection, trauma, other conditions where buformin is unlikely to control the hyperglycemia, renal or hepatic impairment, heart failure, recent myocardial infarct, dehydration, alcoholism, and conditions likely to predispose to lactic acidosis.
Toxicity
[edit]
Buformin was withdrawn from the market in many countries due to an elevated risk of causing lactic acidosis (although not the US, where it was never sold). Buformin is still available and prescribed in Romania (timed release Silubin Retard is sold by Zentiva), Hungary,[13][14][15][16] Taiwan[17] and Japan (sold by Nichi-Iko Pharmaceutical Co., Ltd as "DIBETOS" tablets, each containing 50 mg buformin hydrochloride).[18] The lactic acidosis occurred only in patients with a buformin plasma level of greater than 0.60 μg/mL and was rare in patients with normal renal function.[19][20][21]
In one report, the toxic oral dose was 329 ± 30 mg/day in 24 patients who developed lactic acidosis on buformin. Another group of 24 patients on 258 ± 25 mg/day did not develop lactic acidosis on buformin.[22]
Anticancer properties
[edit]Buformin, along with phenformin and metformin, inhibits the growth and development of cancer.[23][24][25][26][27] The anticancer property of these drugs is due to their ability to disrupt the Warburg effect and revert the cytosolic glycolysis characteristic of cancer cells to normal oxidation of pyruvate by the mitochondria.[28] Metformin reduces liver glucose production in diabetics and disrupts the Warburg effect in cancer by AMPK activation and inhibition of the mTor pathway.[29] Buformin decreased cancer incidence, multiplicity, and burden in chemically induced rat mammary cancer, whereas metformin and phenformin had no statistically significant effect on the carcinogenic process relative to the control group.[30] Buformin also exhibits anti-proliferative and anti-invasive effects in endometrial cancer cells,[31] lung cancer cells[32] and cervical cancer cells.[33]
Antiviral properties
[edit]Biguanides were first noted to be active against influenza in the 1940s.[34] Further studies confirmed their antiviral activity in vitro.[35] Buformin, especially, was potently antiviral against vaccinia and influenza.[36][37][38] Buformin is a metabolic antiviral that inhibits the mTOR pathway used by influenza [39] and Middle East respiratory syndrome-related coronavirus.[40]
History
[edit]Buformin was synthesized as an oral antidiabetic in 1957.[41]
Synthesis
[edit]
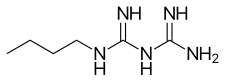
Buformin is obtained by reaction of butylamine and 2-cyanoguanidine.
References
[edit]- ^ Jacker HJ (1964). "[New Pharmacologic Products. 2. Buformin For Oral Therapy Of Diabetes]". Pharmazeutische Praxis. 10: 247–249. PMID 14328846.
- ^ Clarke EG, Berle J (1974). Isolation and identification of drugs in pharmaceuticals, body fluids and post-mortem material. Vol. 1. Pharmaceutical Press, Pharmaceutical Society of Great Britain. Dept. of Pharmaceutical Sciences. p. 226.
- ^ Shroff JR, Bandurco V, Desai R, Kobrin S, Cervoni P (December 1981). "Chemistry and hypoglycemic activity of benzimidoylpyrazoles". Journal of Medicinal Chemistry. 24 (12): 1521–1525. doi:10.1021/jm00144a031. PMID 7310831.
- ^ United States National Library of Medicine ChemLDplus advanced database
- ^ Ravina E, Kubinyi H (2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. Wiley. p. 215.
- ^ Miller RA, Chu Q, Xie J, Foretz M, Viollet B, Birnbaum MJ (February 2013). "Biguanides suppress hepatic glucagon signalling by decreasing production of cyclic AMP". Nature. 494 (7436): 256–260. Bibcode:2013Natur.494..256M. doi:10.1038/nature11808. PMC 3573218. PMID 23292513.
- ^ Beckmann R (March 1968). "The fate of biguanides in man". Annals of the New York Academy of Sciences. 148 (3): 820–832. Bibcode:1968NYASA.148..820B. doi:10.1111/j.1749-6632.1968.tb27755.x. PMID 5241479. S2CID 11875897.
- ^ Beckmann R, Lintz W, Schmidt-Böthelt E (September 1971). "Evaluation of a sustained release form of the oral antidiabetic butylbiguanide (Silubin retard)". European Journal of Clinical Pharmacology. 3 (4): 221–228. doi:10.1007/bf00565010. PMID 5151304. S2CID 39654704.
- ^ Marchetti P, Giannarelli R, di Carlo A, Navalesi R (October 1991). "Pharmacokinetic optimisation of oral hypoglycaemic therapy". Clinical Pharmacokinetics. 21 (4): 308–317. doi:10.2165/00003088-199121040-00006. PMID 1760902. S2CID 11701663.
- ^ Gutsche H, Blumenbach L, Losert W, Wiemann H (1976). "[Concentration of 14C-1-butylbiguanide in plasma of diabetic patients and its elimination after administration of a new Galenical formulation (author's transl)]". Arzneimittel-Forschung. 26 (6): 1227–1229. PMID 989423.
- ^ Ritzl F, Feinendegen LE, Lintz W, Tisljar U (1978). "[Distribution and excretion of 14c-butylbiguanide in man (author's transl)]". Arzneimittel-Forschung. 28 (7): 1184–1186. PMID 582707.
- ^ Kuschinsky G, Lüllmann H (1973). Textbook of pharmacology. Academic Press. p. 225.
- ^ Hankó B, Tukarcs E, Kumli P, Vincze Z (June 2005). "Antidiabetic drug utilization in hungary". Pharmacy World & Science. 27 (3): 263–265. doi:10.1007/s11096-004-5804-1. PMID 16096899. S2CID 9083315.
- ^ Hankó BZ, Reszegi CA, Kumli P, Vincze Z (2005). "[Practice of antidiabetic therapy in Hungary]". Acta Pharmaceutica Hungarica (in Hungarian). 75 (2): 77–86. PMID 16318232.
- ^ Schlesser JL (1990). Drugs available abroad. Gale Research Inc.; Derwent Publications, Ltd. p. 28.
- ^ Verdonck LF, Sangster B, van Heijst AN, de Groot G, Maes RA (1981). "Buformin concentrations in a case of fatal lactic acidosis". Diabetologia. 20 (1): 45–46. doi:10.1007/BF01789112. PMID 7202882.
- ^ Chou CH, Cheng CL, Huang CC (May 2004). "A validated HPLC method with ultraviolet detection for the determination of buformin in plasma". Biomedical Chromatography. 18 (4): 254–258. doi:10.1002/bmc.312. PMID 15162388.
- ^ Wurita A, Hasegawa K, Nozawa H, Yamagishi I, Minakata K, Watanabe K, Suzuki O (September 2020). "Postmortem distribution/redistribution of buformin in body fluids and solid tissues in an autopsy case using liquid chromatography-tandem mass spectrometry with QuEChERS extraction method". Forensic Science International. 314: 110376. doi:10.1016/j.forsciint.2020.110376. PMID 32615395. S2CID 220328342.
- ^ Wittmann P, Haslbeck M, Bachmann W, Mehnert H (January 1977). "[Lactic acidosis in diabetics on biguanides (author's transl)]". Deutsche Medizinische Wochenschrift (in German). 102 (1): 5–10. doi:10.1055/s-0028-1104832. PMID 11984. S2CID 260117450.
- ^ Berger W, Mehnert-Aner S, Mülly K, Heierli C, Ritz R (December 1976). "[10 cases of lactic acidosis during biguanide therapy (buformin and phenformin)]". Schweizerische Medizinische Wochenschrift. 106 (50): 1830–1834. PMID 1013709.
- ^ Deppermann D, Heidland A, Ritz E, Hörl W (September 1978). "[Lactic acidosis--a possible complication in buformin-treated diabetics (author's transl)]". Klinische Wochenschrift. 56 (17): 843–853. doi:10.1007/BF01479834. PMID 713413. S2CID 39728557.
- ^ Luft D, Schmülling RM, Eggstein M (February 1978). "Lactic acidosis in biguanide-treated diabetics: a review of 330 cases". Diabetologia. 14 (2): 75–87. doi:10.1007/bf01263444. PMID 344119.
- ^ Saito S, Furuno A, Sakurai J, Sakamoto A, Park HR, Shin-Ya K, et al. (May 2009). "Chemical genomics identifies the unfolded protein response as a target for selective cancer cell killing during glucose deprivation". Cancer Research. 69 (10): 4225–4234. doi:10.1158/0008-5472.can-08-2689. PMID 19435925.
- ^ Anisimov VN (October 2003). "Insulin/IGF-1 signaling pathway driving aging and cancer as a target for pharmacological intervention". Experimental Gerontology. 38 (10): 1041–1049. doi:10.1016/s0531-5565(03)00169-4. PMID 14580857. S2CID 27811309.
- ^ Alexandrov VA, Anisimov VN, Belous NM, Vasilyeva IA, Mazon VB (1980). "The inhibition of the transplacental blastomogenic effect of nitrosomethylurea by postnatal administration of buformin to rats". Carcinogenesis. 1 (12): 975–978. doi:10.1093/carcin/1.12.975. PMID 11272113.
- ^ Anisimov VN, Ostroumova MN, Dil'man VM (June 1980). "[Inhibition of the blastomogenic effect of 7,12-dimethylbenz(a)anthracene in female rats by buformin, diphenin, a polypeptide pineal extract and L-DOPA]". Biulleten' Eksperimental'noi Biologii I Meditsiny. 89 (6): 723–725. doi:10.1007/bf00836263. PMID 6772259. S2CID 46058518.
- ^ Anisimov VN, Berstein LM, Popovich IG, Zabezhinski MA, Egormin PA, Tyndyk ML, et al. (December 2005). "Central and peripheral effects of insulin/IGF-1 signaling in aging and cancer: antidiabetic drugs as geroprotectors and anticarcinogens". Annals of the New York Academy of Sciences. 1057 (1): 220–234. Bibcode:2005NYASA1057..220A. doi:10.1196/annals.1356.017. PMID 16399897. S2CID 5744858.
- ^ Vander Heiden MG, Cantley LC, Thompson CB (May 2009). "Understanding the Warburg effect: the metabolic requirements of cell proliferation". Science. 324 (5930): 1029–1033. Bibcode:2009Sci...324.1029V. doi:10.1126/science.1160809. PMC 2849637. PMID 19460998.
- ^ Shaw RJ, Lamia KA, Vasquez D, Koo SH, Bardeesy N, Depinho RA, et al. (December 2005). "The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin". Science. 310 (5754): 1642–1646. Bibcode:2005Sci...310.1642S. doi:10.1126/science.1120781. PMC 3074427. PMID 16308421.
- ^ Zhu Z, Jiang W, Thompson MD, Echeverria D, McGinley JN, Thompson HJ (June 2015). "Effects of metformin, buformin, and phenformin on the post-initiation stage of chemically induced mammary carcinogenesis in the rat". Cancer Prevention Research. 8 (6): 518–527. doi:10.1158/1940-6207.CAPR-14-0121. PMC 4452421. PMID 25804611.
- ^ Kilgore J, Jackson AL, Clark LH, Guo H, Zhang L, Jones HM, et al. (2016). "Buformin exhibits anti-proliferative and anti-invasive effects in endometrial cancer cells". American Journal of Translational Research. 8 (6): 2705–2715. PMC 4931164. PMID 27398153.
- ^ Yakisich JS, Azad N, Kaushik V, Iyer AK (2019). "The Biguanides Metformin and Buformin in Combination with 2-Deoxy-glucose or WZB-117 Inhibit the Viability of Highly Resistant Human Lung Cancer Cells". Stem Cells International. 2019: 6254269. doi:10.1155/2019/6254269. PMC 6409035. PMID 30918522.
- ^ Li J, Chen L, Liu Q, Tang M, Wang Y, Yu J (June 2018). "Buformin suppresses proliferation and invasion via AMPK/S6 pathway in cervical cancer and synergizes with paclitaxel". Cancer Biology & Therapy. 19 (6): 507–517. doi:10.1080/15384047.2018.1433504. PMC 5927663. PMID 29400636.
- ^ Bailey CJ (September 2017). "Metformin: historical overview". Diabetologia. 60 (9): 1566–1576. doi:10.1007/s00125-017-4318-z. PMID 28776081. S2CID 2088719.
- ^ Weinberg ED (March 1968). "Antimicrobial activities of biguanides". Annals of the New York Academy of Sciences. 148 (3): 587–600. Bibcode:1968NYASA.148..587W. doi:10.1111/j.1749-6632.1968.tb27733.x. PMID 4872309. S2CID 19580586.
- ^ Fara GM, Lugaro G, Galli MG, Giannattasio G (April 1974). "Antiviral activity of selected biguanide derivatives". Pharmacological Research Communications. 6 (2): 117–126. doi:10.1016/s0031-6989(74)80019-6. PMID 4373765.
- ^ Denys A, Bocian J (March 1970). "[Effect of Silubin-retard (1-butyl-biguanide hydrochloride) on the course of influenza-virus infection in mice]". Polski Tygodnik Lekarski (in Polish). 25 (9): 332–334. PMID 5447272.
- ^ Babiński S, Giermaziak H (November 1973). "[Influenza epidemic in 1971 in diabetics treated with 1-butyl-biguanidine hydrochloride (Silubin retard) and 1-phenylethyl-biguanidine hydrochloride (Phenformin)]". Polski Tygodnik Lekarski (in Polish). 28 (46): 1815–1817. PMID 4771858.
- ^ Lehrer S (May 2020). "Inhaled biguanides and mTOR inhibition for influenza and coronavirus (Review)". World Academy of Sciences Journal. 2 (3). doi:10.3892/wasj.2020.42. PMC 7170270. PMID 32313883.
- ^ Kindrachuk J, Ork B, Hart BJ, Mazur S, Holbrook MR, Frieman MB, et al. (February 2015). "Antiviral potential of ERK/MAPK and PI3K/AKT/mTOR signaling modulation for Middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis". Antimicrobial Agents and Chemotherapy. 59 (2): 1088–1099. doi:10.1128/AAC.03659-14. PMC 4335870. PMID 25487801.
- ^ US 2961377, Shapiro SL, Freedman L, "Salts Of N-Amylbiguanide.", issued 1960, assigned to US Vitamin and Pharmaceutical Corp
- ^ Shapiro SL, Parrino VA, Freedman L (1959). "Hypoglycemic Agents. III.1—3N1-Alkyl- and Aralkylbiguanides". Journal of the American Chemical Society. 81 (14): 3728–3736. doi:10.1021/ja01523a060.
